Abstract
Background
For many patients with hematologic malignancies, hematopoietic cell transplantation (HCT) remains the best and possibly only potentially curative option. However, despite more than 40 million donors registered globally, many patients who need unrelated donor (URD) HCT still cannot identify an 8/8 matched URD. The use of mismatched unrelated donors (MMUD) could alleviate this problem, but historical survival rates are lower when using grafts from MMUD and conventional calcineurin inhibitor based GVHD prophylaxis.
The National Marrow Donor Program (NMDP) recently reported the results of a prospective, phase II multi-center clinical trial (15-MMUD), which assessed the safety and efficacy of MMUD (4/8-7/8) HCT using the post-transplant cyclophosphamide (PTCy) graft-versus-host disease (GVHD) prophylaxis backbone (Shaw et al. JCO 2021). The study enrolled 80 patients and achieved its primary endpoint with 1-year overall survival (OS) of 76%. OS did not differ by HLA match grade or conditioning intensity, and 39% of recipients had donors matched at <7/8 level.
Notably, 48% of the patients in the 15-MMUD study were racial/ethnic minorities. Such patients have long faced disparities in key HCT aspects: transplant access, post-HCT outcomes(Majhail et al. BMT 2012) and low enrollment in clinical trials (Williams et al. BMT 2020).
The 15-MMUD study limited the donor graft source to bone marrow (BM) and did not include children. The ACCESS study is now evaluating the use of MMUD PBSC in adults while exploring the safety and efficacy of MMUD BM in pediatric patients who may lack other donor options.
Study Design and Methods
ACCESS (NCT04904588) is an NMDP-sponsored multi-center phase II study with three strata - 2 adult strata based on conditioning intensity [Stratum 1 - myeloablative (MAC), or Stratum 2 -reduced intensity (RIC)] and a pediatric stratum. All patients receive PTCy on days 3 and 4 post-HCT, tacrolimus, and MMF. Key inclusion criteria include hematological malignancy as underlying disease and HCT-CI score of 4 or less in the adult MAC stratum. Exclusion criteria include availability of a suitable HLA-matched related or 8/8 high resolution matched URD and the presence of donor-specific HLA antibodies to any mismatched allele/antigen with mean fluorescence intensity > 3000. URD must be 18-35 years old and matched at 4/8-7/8 alleles (HLA-A, -B, -C, and -DRB1).
The primary endpoint is one-year OS. Select secondary and exploratory endpoints include GVHD-Relapse Free Survival (GRFS) and event-free survival (EFS) at 1-year, incidence of patient-reported toxicities and symptoms, OS in the pediatric stratum, and the prioritization of donor characteristics used by centers in URD selection.
The study will accrue 180 subjects (140 adults, 70/stratum; 40 pediatrics) to determine whether OS at one-year is 75% in the adult strata with a margin of error +/- 10%. Stopping rules include severe acute GVHD, graft failure, non-relapse mortality, and cytokine release syndrome.
Study Accrual and Subject Characteristics
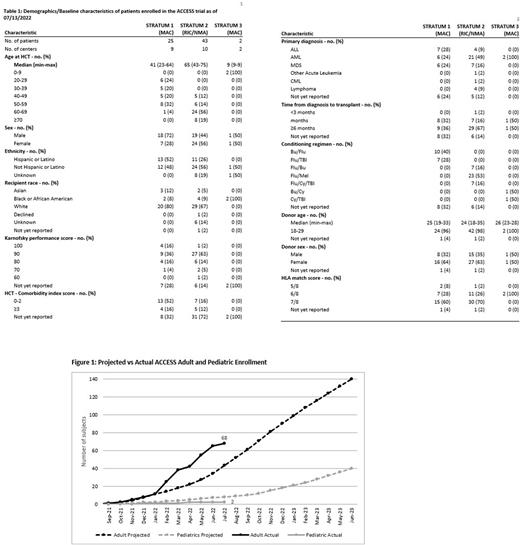
26 of approximately 40 planned study sites are open to enrollment, 16 of which have consented or enrolled at least one subject. Demographics as of 7/13/22 are presented in Table 1. Adult accrual has exceeded projections to date and is over 150% of projected accrual, while pediatric accrual is behind target (Figure 1).
Consistent with the 15-MMUD study, 53% of enrolled patients are racially/ethnically diverse, and 36% have received a <7/8 mismatched graft. AML has been the most common diagnosis. Chemotherapy-based conditioning regimens have been used more often than TBI-containing regimens, Busulfan/Fludarabine on Stratum 1 (40%) and Fludarabine/Melphalan on Stratum 2 (53%). 89% of the reported infused products to adult patients have been cryopreserved. Unrelated donor HLA match score has included 7/8 (64%), 6/8 (29%), and 5/8 (4%) matched donors, with 7 study sites selecting a donor that is <7/8 matched. Registry models conducted in support of the study suggest that all patients will have multiple donor options available considering matching at > 5/8.
Future Directions
Accrual has been brisk and site participation broad, suggesting ACCESS addresses an unmet patient need. Adult accrual is anticipated to complete in mid-2023, with 1 year of follow-up for all subjects. Thus, planning for the next NMDP-sponsored MMUD study which will focus on further mitigating risk of NRM and GVHD has begun.
Disclosures
Al Malki:NexImmune: Consultancy, Research Funding; Hasna Biopharma: Membership on an entity's Board of Directors or advisory committees; Miltenyi Biotec: Consultancy, Research Funding; Incyte: Consultancy, Research Funding; CareDx: Consultancy, Research Funding; Gilead: Consultancy, Research Funding. Devine:Orca Bio: Consultancy, Other: Payment to NMDP for consulting. Shaw:OrcaBio: Consultancy; Mallinkrodt: Consultancy. Qayed:Vertex: Honoraria; Novartis: Honoraria. Auletta:AscellaHealth: Membership on an entity's Board of Directors or advisory committees. Stefanski:Novartis: Other: Ad Board, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal